Inside a Michigan COVID-19 ward: Younger patients, familiar sadness and politics
Andrea Kanerva sat on the edge of the bed with her hair pulled up, exposing the ties of her blue hospital gown. Fuzzy green socks with white treads covered her feet.
She spoke deliberately, breathing deeply as the lines on the monitor behind her danced up and down, graphing fluctuations in Kanerva’s pulse, blood-oxygen level and respiratory rate.
Kanerva, who lives in Hamburg Township and works as a service adviser for Briarwood Ford in Saline, is part of Michigan’s third wave of novel coronavirus patients — hospitalized at the height of a surge that for weeks has led the nation.
“There were days when I thought I was turning around a little bit and then I went right back down. It’s been a long struggle,” said Kanerva, who tested positive for the virus on April 7 and was hospitalized nine days later.
The day she went to the emergency room — April 16 — Michigan’s third COVID-19 surge peaked, hitting the highest number of new cases in a single day this year — 8,955. Coronavirus hospitalizations topped 4,000 that day, too — a more than 460% rise from four weeks earlier.
She was admitted to St. Joseph Mercy Ann Arbor Hospital and needed supplemental oxygen to breathe.
By Tuesday morning, doctors weaned Kanerva off the oxygen to assess whether she could remain stable without it and potentially go home.
“I’m really looking forward to it,” she said. “It’ll be nice to be in my own home, hopefully, sit on my couch and rest. I don’t really foresee doing a whole lot. But that’s all right. I’ll take one step at a time and do what I can.”
There are some stark differences in the state’s third surge compared with previous spikes, said Dr. David Vandenberg, vice president and chief medical officer of St. Joseph Mercy Ann Arbor.
“What we’re seeing is a definite shift of toward the younger patients,” he said. “No question about that. I would say that our average age … is about 58 in this surge.”
Kanerva, a mother and grandmother of three, is 59.
The downward shift in the age of patients this time, Vandenberg said, is likely due to how vaccines were prioritized in the state, with more doses initially aimed at older, more vulnerable people.
Statewide, about 65% of residents ages 65 and older are fully vaccinated — about 1.1 million people, according to the Michigan COVID-19 vaccine dashboard. That compares with about 40% of Michiganders ages 50-64; 24% of those ages 40-49, and 21% of those ages 30-39.
The vast majority of people contracting the virus now and getting sick enough to be hospitalized haven’t yet gotten a COVID-19 vaccine, Vandenberg said.
“We have definitely seen several very sick 20-somethings and 30-somethings, 40-somethings,” he said.
Kanerva is among the unvaccinated.
“I was trying to get the vaccine, and I got sick before there was a place available for me to get it,” she said. “I will definitely be doing that. I’ll tell you that. I would recommend to anybody to definitely get it because this is not a fun thing.”
Of the 15 coronavirus patients on ventilators at St. Joseph Mercy last week, seven were in their 30s or 40s, Vandenberg said.
“Most of those patients have some comorbidities,” which are underlying diseases that put them at higher risk for severe illness or death from COVID-19, and can include such conditions as obesity, diabetes and high blood pressure, he said. “We’re definitely seeing a younger age group who’s pretty sick.”
“Thank God,” Kanerva said, she never needed a ventilator. “I sure didn’t want that.
“I was on 3 liters (of oxygen) for quite a while … between 3 and 4,” she said. “Yesterday, they took me down a little bit, and then today, I haven’t had any. I’ve been doing good.”
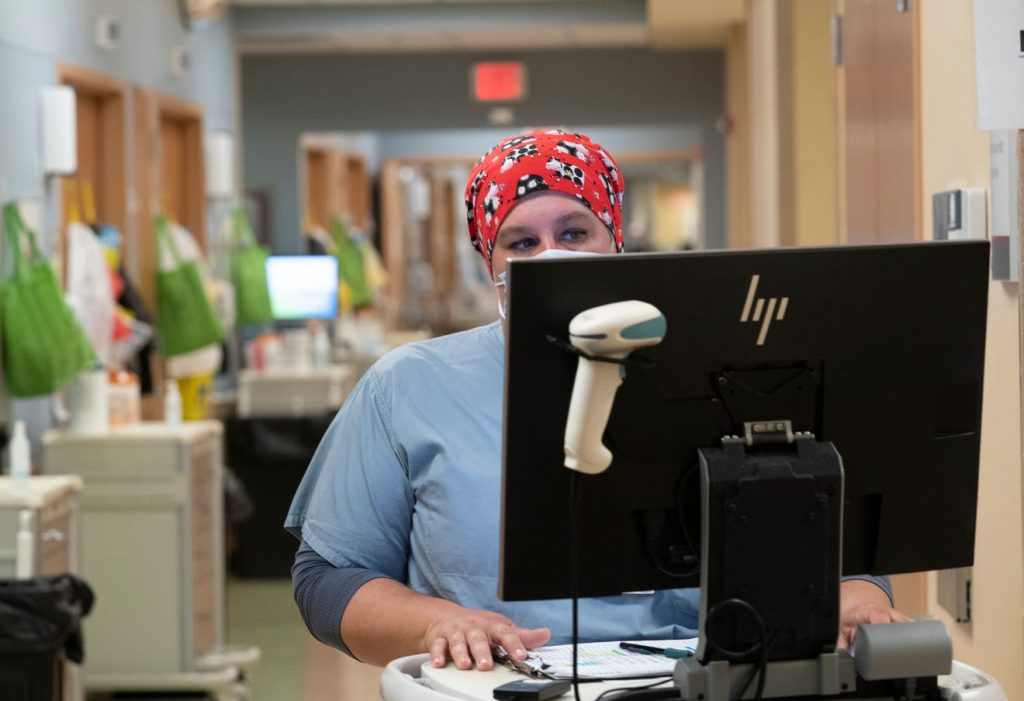
After the first two waves of COVID-19 patients who poured into the hospital in March-April of 2020 and again in November and December, registered nurse Karla Kanitz thought she’d seen it all.
She’s the charge nurse for the 32-bed 10th floor east unit at St. Joseph Mercy Ann Arbor, where every room can convert into a negative-pressure room, ideal for containing infectious diseases like novel coronavirus; each room can serve in an intensive-care capacity, too.
Last week, the unit was filled with coronavirus patients. Two other floors of the hospital also were functioning as COVID-19 units.
In the early days of the pandemic, Kanitz recalled, “we didn’t have a lot of PPE. We didn’t have a lot of staff. We didn’t have a lot of anything. We didn’t know what we were dealing with.
“I got COVID myself … and that was a scary time, you know?”
But this third round — with high case rates driven by a more contagious and potentially more deadly strain, known as the B.1.1.7 or United Kingdom variant — has delivered plenty of new surprises for the 19-year veteran.
Source: Detroit Free Press